Combined lipid-lowering therapy
Post updated: July 11
Cardiovascular disease (CVD) is the leading cause of death worldwide. Prescribing statins for primary and secondary prevention of CVD reduces the risk of adverse cardiovascular events by lowering low-density lipoprotein cholesterol (LDL-C). However, in some clinical cases, despite the use of high-dose statin therapy, patients have residual cardiovascular risks, in particular due to the lack of efficacy of monotherapy. An alternative for for this cohort of patients may be a combination of statins and ezetimibe.
It is known that CVD is the leading cause of death worldwide [1]. In particular, in 2019, among the total of 56.5 million deaths, 32.8% (18.6 million) were due to CVD. CVD-related deaths, which is 17.8% (10.1 million) higher than deaths from tumours [2]. The most common causes of death from CVD include coronary heart disease (2.0%; 1.2 million) and hypertension [2].
Risk factors for developing CVD
Metabolic, behavioural, environmental and occupational
risk factors have a negative impact on the development
and progression of CVD [1, 3-6]. High systolic
blood pressure, diet, and LDL cholesterol levels are among the
are the main risk factors for CVD, accounting for 25.0;
17.2 and 11.0% of CVD deaths, respectively [2].
Target LDL cholesterol levels
Most patients with dyslipidaemia do not achieve
optimal LDL cholesterol levels by changing
lifestyle changes and taking affordable and accessible
statins [7-11]. Thus, according to the multicentre
DA VINCI study, only 33% of 5888 patients
with dyslipidaemia reached the target LDL-C level,
recommended by the European Society of Cardiology (ESC).
Society (ESC, 2019) [12]. In different European countries, a similar trend is observed.
There is a similar trend in different European countries [13-15]. The data of the Australian
Australian study involving 61,407 patients
showed that only 36% of participants reached
the recommended levels of LDL-C [16]. Analysing data from 44 million US residents.
analysing data from 44 million US residents, only 36% of patients
with a high risk of CVD had the recommended level of
LDL-C <70 mg/dL (~1.8 mmol/L) [17].
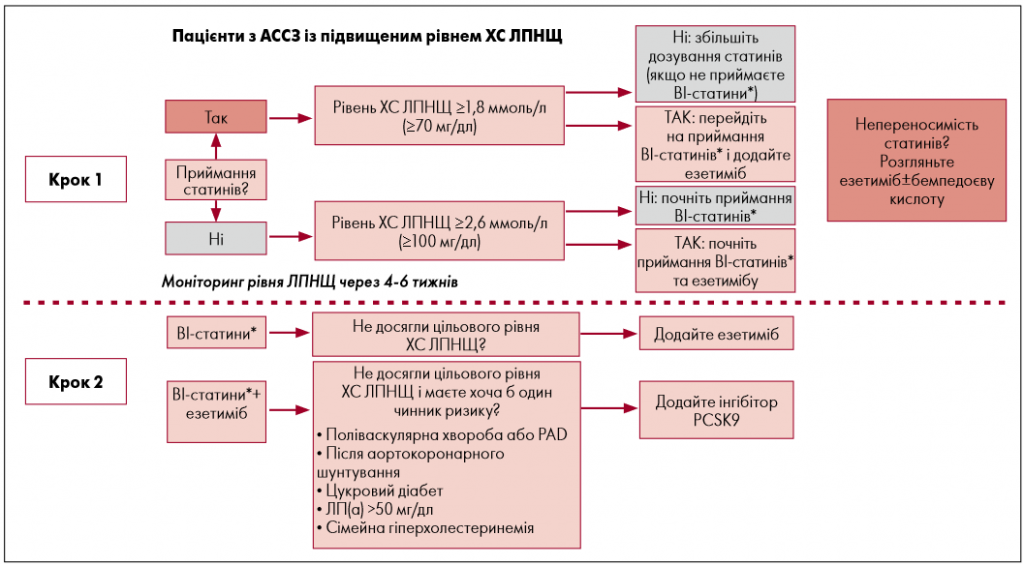
There are several reasons why most patients do not achieve the required LDL-C levels. Firstly, according to the recommendations of the European to the recommendations of the European Society of Cardiology Society (ESC, 2019) and the leading US cardiology associations of the American Society of Cardiology / American College of Cardiology. American College of Cardiology (AHA/ACC, multi-society 2018) - it is necessary to achieve a more significant LDL cholesterol reduction, in accordance with the principle of "the lower the better" [18-20]. For example, the target LDL-C levels for high-risk patients was reduced to <1.8 mmol/l. Secondly, there is a simple is the lack of interest of patients in reducing their LDL-C levels. LDL-C levels through lifestyle changes or regular pharmaceutical treatment. pharmacological treatment due to insufficiently fast results.
An additional obstacle may also be the high prices of new drugs, such as PCSK9 inhibitors, which that need to be taken to quickly achieve the goals of treatment goals. Given that 9.1% of patients are intolerance to statins, alternative approaches to to lowering cholesterol may not be enough.
Drugs for the correction of dyslipidaemia
The ESC (2019) and AHA/ACC/multi
society (2018) provide a list of pharmaceutical preparations
drugs that can be used to lower blood
lipids in the blood and reduce the risk of CVD in patients
with dyslipidaemia (Table).
According to these guidelines, statins are the first line of therapy for primary and secondary prevention of CVD prevention of CVD in patients with hypercholesterolaemia and hyper triglyceridemia.
The mechanism of action of statins
Statins help to reduce the synthesis of cholesterol
in the body by competitively inhibiting the enzyme
3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA)
reductase [19]. Reducing the synthesis of cholesterol in the liver
in the liver leads to an increase in the surface expression of
of LDL-C receptors, which, in turn, increases
LDL cholesterol absorption, leading to a decrease in
of LDL-C, ApoB-100 and triglycerides in the blood serum.
blood. Due to competitive inhibition of HMG-CoA,
the dose-dependent effectiveness of statins is used
in clinical practice to escalate treatment from low- to
to high-intensity statin therapy for patients at risk.
therapy for patients at risk. It is known that statins
low/medium intensity statins are known to reduce
LDL cholesterol by 30-50% and triglycerides by 20%, while
while high intensity statins - by >50 and 40%, respectively [19,
31]. At the same time, statins can increase the level of cholesterol
sterol of high-density lipoprotein (HDL)
levels by 10%, depending on the dose [32].
According to studies, in patients treated with statins
statins, no significant increase in the level of
lipoprotein (a) [Lp(a)] [33, 34].
| Name | MoA | Type | RoA | LDL CHOLESTEROL | TG | MACE |
|---|---|---|---|---|---|---|
| Statins of low / medium intensity | Inhibition of HMG-CoA reductase, pleiotropic | Pills | Once a day, p.a. | -30% | -20% | -22% |
| High-intensity statins | Inhibition of HMG-CoA, pleiotropic | Pills | Once a day, p.a. | -50% | -40% | -15% а |
| Ezetimibe | Inhibition NPC1L1 | Pills | Once a day, p.a. | -24% | -12% | -6% |
| Evolocumab | Inhibition PCSK9 | Injections | Раз на 2 тижні/ щоміÑÑцÑ, п.Ñ. | -60% | -26% | -15% |
| Alirocumab | Inhibition PCSK9 | Injections/td> | Once every 2 weeks/ monthly, p.p. | -60% | -26% | -15% |
| Fibrates | Activation PPARa | Pills | Once a day, p.a. | -20% | -50% | -10% |
| Icosapent ethyl | Reduction of TG levels, pleiotropic | Pills | Twice a day, p.o. | -6% | -20% | -25% |
| Note. a The reported reduction in MACE for high intensity statins refers to the additional benefit compared with low/medium intensity statins. HMG-CoA - 3-hydroxy-3-methylglutaryl coenzyme A, LDL-C - low-density lipoprotein cholesterol (LDL-C), MACE - major adverse cardiovascular events. MoA mechanism of action, NPC1L1 - Niemann-Pick C1-like protein, PCSK9 - proprotein convertase subtilisin-kexin type 9, PO (p.o.) - oral oral, PPAR-α - peroxisome proliferator-activated receptor alpha, RoA - route of administration, SC - subcutaneously, TG(TG) - triglycerides. Adapted from D. T. Michaeli, 2023. | ||||||
In addition to changes in blood lipid levels, the results of in vitro and in vivo studies have confirmed that statins have beneficial cardioprotective pleiotropic effects, such as Improvement of endothelial dysfunction, increased bioavailability of nitric oxide; antioxidant properties properties, suppression of inflammatory reactions and stabilisation of atherosclerotic plaques [35, 36]. However, the significance of of these pleiotropic effects in clinical practice is still remains controversial [37].
Effectiveness of statins
For the prevention of CVD, the effectiveness of statins is confirmed
is confirmed by meta-analyses [38-50]. Thus, analysing
data from 170 thousand patients, a reduction in LDL-C was found
by 38.67 mg/dl (1 mmol/l), which is associated with a reduction in
the risk of major cardiovascular events (MACE)
by 22% (95% CI -20 to -24; p<0.0001) during therapy
with low/moderate intensity statins [38].
This confirms that LDL-C levels are a reliable surrogate parameter for clinical endpoints. surrogate parameter for the clinical endpoints of MACE and cardiac death. clinical endpoints of MACE and cardiovascular death. Further intensification of therapy provided an additional 15% reduction in MACE risk. MACE risk by 15% (95% CI -11 to -18; p<0,0001) [38]. The results are consistent with data from cohorts of primary and secondary prevention prevention [40, 41, 48, 49, 51]. In patients with low risk of CVD (<10%), statin therapy helped to reduce the risk of the risk of serious vascular events (RR 0.79; 95% CI 0.77-0.81 per 1.0 mmol/l LDL-C reduction) regardless of previous vascular disease [40]. Thanks to statin therapy, the risk of all-cause mortality events was reduced by 9% for every 1.0 mmol/l reduction in Since statins are metabolised in the liver, inhibitors of inhibitors and inducers of the cytochrome P450 system (CYP) system, in particular antimicrobials, calcium antagonists calcium antagonists, cyclosporine and grapefruit juice, may lead to drug-drug interactions, which may affect their bioavailability. on their bioavailability, and ultimately, on an increase in side effects or restriction of side effects or limitation of therapeutic effect.
Thus, according to a recent meta-analysis of 176 studies involving 4.1 million patients, 9.1% of people were intolerant of statins. intolerance to statins [25]. Age, female sex, Asian and black (equatorial) races, obesity, diabetes mellitus diabetes mellitus, hypothyroidism, chronic liver disease, renal failure, antiarrhythmic drugs, calcium channel blockers calcium channel blockers, alcohol consumption and high doses of statins. high doses of statins were associated with a higher risk of of statin intolerance [25]. Despite the fact that statins are first-line drugs for the correction of dyslipidaemia, in particular, in people with hypercholesterolaemia or hypertriglycerolaemia. ceridaemia, many patients have blood lipid levels remains above the target levels set by the ESC (2019). levels. Over the past two decades, scientists have been actively have been actively working on the development of new pharmacological treatment of CVD to reduce the risk of adverse cardiovascular events. of adverse cardiovascular events among patients at risk group. In fact, modern means of such therapy are recommended are recommended as an adjuvant to medium/high intensity statins or as monotherapy drugs. intensity statins or as monotherapy drugs in patients with statin intolerance.
Effect of ezetimibe on dyslipidaemia
Ezetimibe selectively inhibits the absorption of chol
sterol in the small intestine, without changing the absorption of other
absorption of other nutrients and vitamins [56,
57]. The molecular target of ezetimibe is the carrier of
Niemann-Pick C1-Like 1 (NPC1L1), which is responsible for the absorption of
responsible for the absorption of cholesterol and phytosterols
in the intestine. The data from the genetic sequencing study
(involving more than 90 thousand patients) confirmed
significantly lower LDL cholesterol levels and a lower risk of coronary heart disease
coronary heart disease in patients with NPC1L1 mutations [58].
According to studies, compared to monotherapy with statins statins, their combination with ezetimibe reduced the level of LDL cholesterol by 24%, ApoB-100 by 14%, triglycerides by 12% and high-sensitivity C-reactive protein (hsCRP) by 13% [59-61]. According to the results of a of the randomised, controlled, double-blind IMPROVE-IT trial, which included 18,144 patients after acute coronary patients after acute coronary syndrome with a follow-up of 6 years. ezetimibe, which was added to simvastatin, was shown to be more effective than simvastatin added to simvastatin, compared with monotherapy simvastatin monotherapy reduced the risk of MACE by 6% (95% CI 1 to 11; p=0.016).
The ENHANCE study did not confirm that the addition of ezetimibe to statins of ezetimibe to statins significantly reduces the thickness of the intima and media thickness in patients with familial hypercholesterolaemia. although the results of the SHARP and SEAS trials showed the efficacy of ezetimibe. studies showed the effectiveness of ezetimibe in the prevention of ischaemic cardiovascular events [62-65]. Safety and efficacy of ezetimibe have also been confirmed by numerous meta-analyses. meta-analyses [61, 66-70].
In particular, the EWTOPIA-75 study investigated the efficacy of ezetimibe monotherapy for primary cardiovascular prevention in patients aged >75 years of age. To receive ezetimibe (10 mg daily) 3796 patients were randomly assigned to receive ezetimibe (mg daily) to to compare the effect with conventional treatment. After a median follow-up period of 4.1 years ezetimibe reduced the incidence of MACE by 34% (RR 0.2, 95%). (HR 0.66; 95% CI 0.50-0.86; p=0.002) [71]. Compared with statin monotherapy, adjuvant therapy with ezeti did not increase the incidence of side effects and did not lead to discontinuation of effects and did not lead to treatment discontinuation.
Conclusions
In order to prevent cardiovascular events, international research groups are now
international research teams are actively working on the development of new drugs
of new drugs that will help to effectively
lipoprotein levels. Combination therapy
is widely used to treat arterial hypertension.
hypertension and, more recently, dyslipidaemia. The main goal
of developing a combination of drugs is to increase
the effectiveness of therapy by minimising the frequency of undesirable side effects and
undesirable side effects and improving patient adherence.
of the patient to treatment. According to S.R. Gnanenthiran et al.
(2023), combination therapy with drugs with fixed
doses of active substances in one tablet (single-pill)
may help to complement and improve existing
strategies to reduce overall CVD risk.
A combination drug of rosuvastatin and ezetimibe is now available on the Ukrainian pharmaceutical market of rosuvastatin and ezetimibe is represented by the drug Rosulip® Plus (manufactured by "PHARMACEUTICAL PLANT EGIS). The recommended daily dose of the drug is one capsule (containing 10 mg of rosuvastatin and 10 mg of ezetimibe or 20 mg of rosuvastatin and 10 mg of ezetimibe), which should be taken taken regardless of food intake. Rosulip® Plus is the drug of choice for combination therapy. Rosulip® Plus is the drug of choice for combination therapy. for lipid-lowering therapy. The therapeutic effect is observed within 1 week after the start of treatment, in 2 weeks it reaches 90% of the possible, and after 4 weeks - the maximum level.