A very high-risk patient in secondary prevention
Post updated: July 18
Consider the real medical situation from The Clinician's Handbook.
CASE1. A very high-risk patient in secondary prevention.
Recall! The cases are based on real cases and clinical experience.
Background data
The patient is a 60–year-old entrepreneur, married, has three adult children. He has been smoking 10 cigarettes a day for many years. I came to the hospital for a health check at the insistence of my wife.
What do we need to know to assess its risk?
Medical history
The patient suffered a subendocardial myocardial infarction (MI) 5 years ago. He was sent under the supervision of his therapist, but was not observed. He is currently not taking medication and has no family history of early cardiovascular disease. There is no history of chest pain.
Risk factors
Smoker, body mass index (BMI) 29 kg/m2, waist circumference 105 cm, low physical activity.
Physical status: moderate abdominal obesity. There is no Xanthe. Auscultation of the heart is normal. Arterial pressure (BP) is 145/90 mmHg. Peripheral blood circulation is normal.
Laboratory tests
There were no signs of the previous one on the ECG.
TC 5.2 mmol/L (200 mg/dl)
TG 2.2 mmol/L (193 mg/dl)
HDL CHOLESTEROL 1.0 mmol/L (38 mg/dl)
LDL CHOLESTEROL 3.2 mmol/l (123 mg/dl)
Blood glucose 6.9 mmol/l (124 mg/dl); Lp(a) 200 mg/dl.
What risk category does the patient belong to?
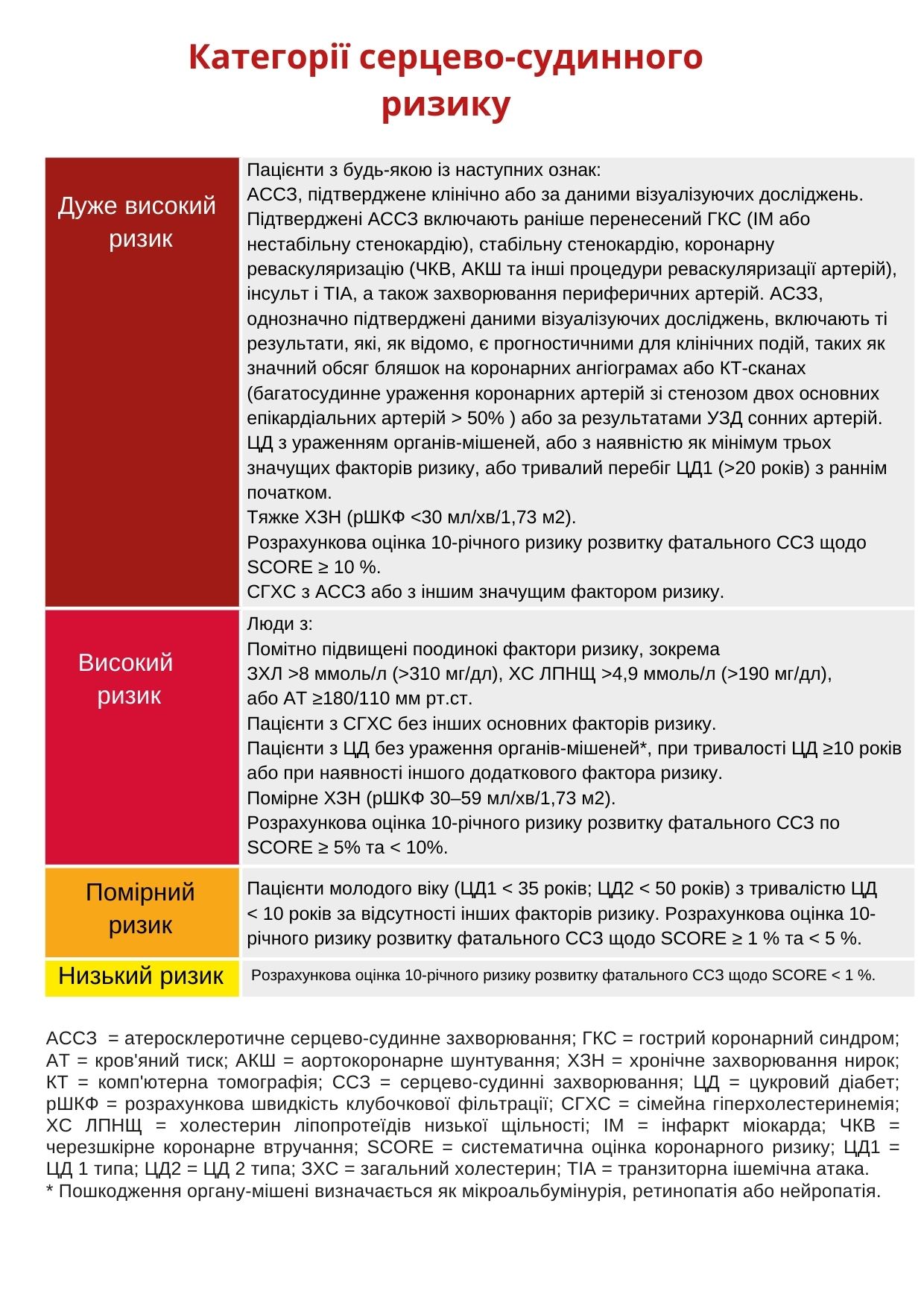
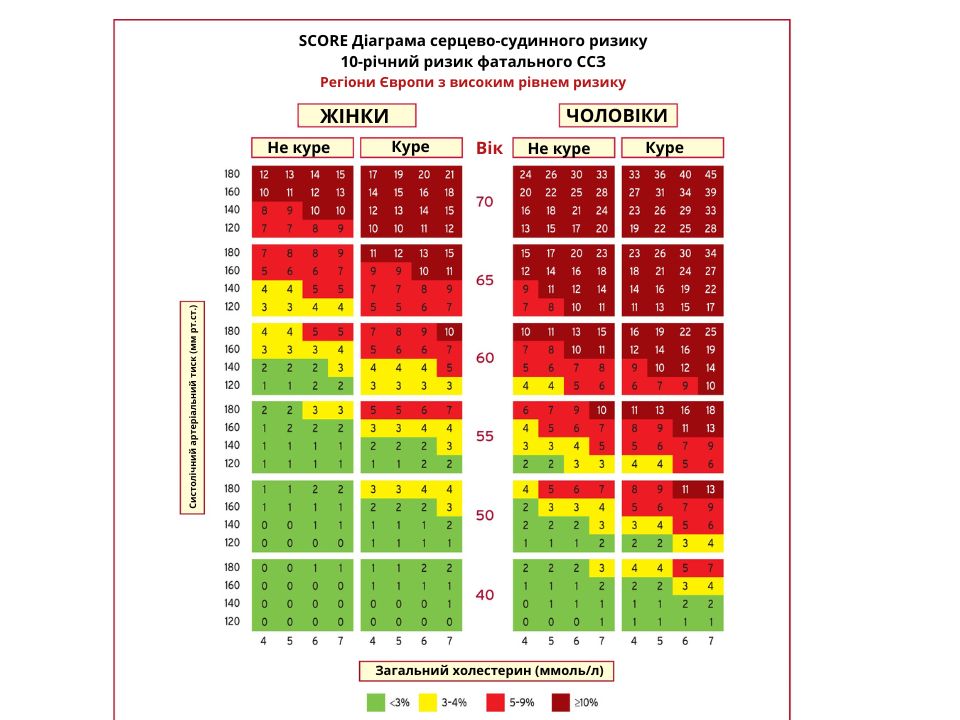
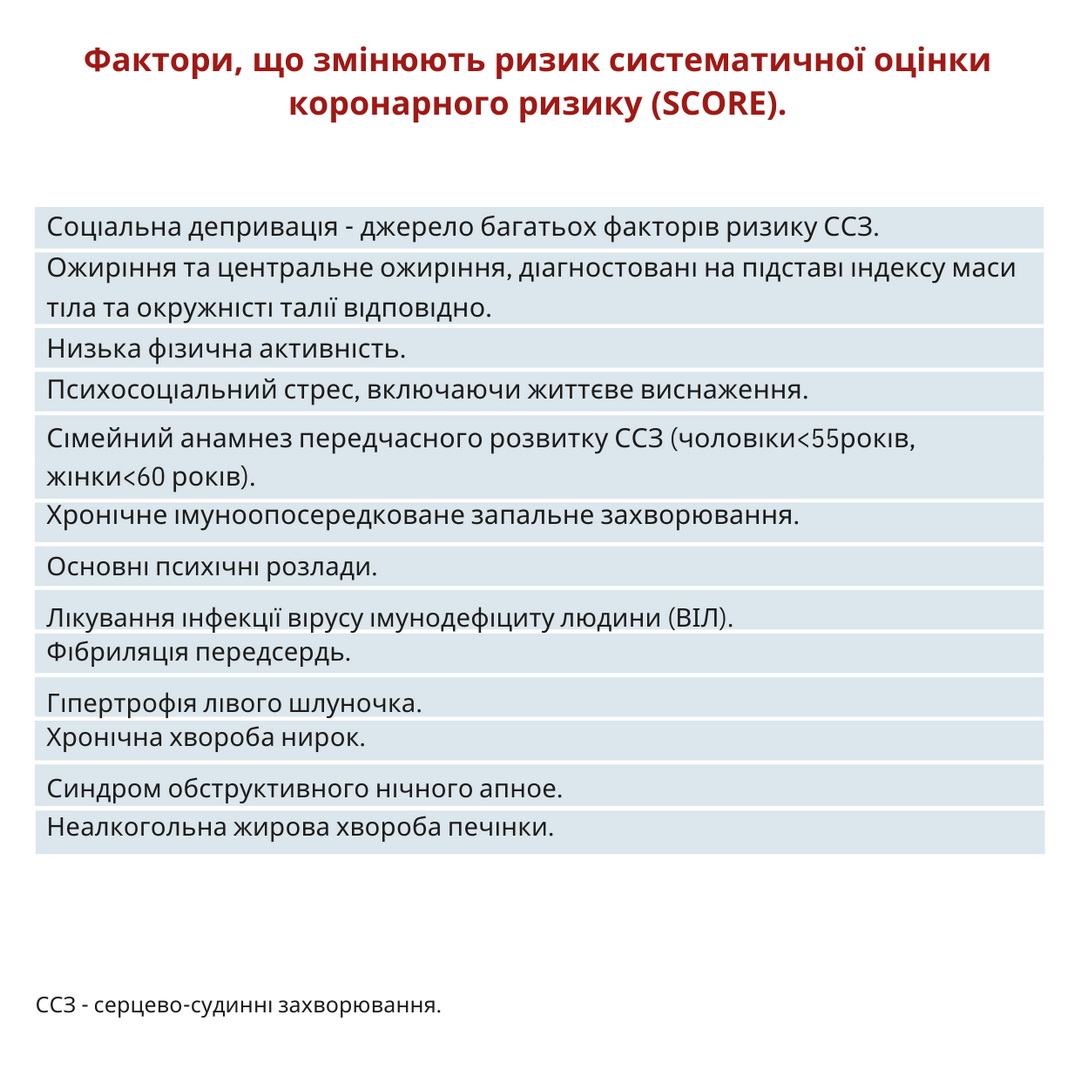
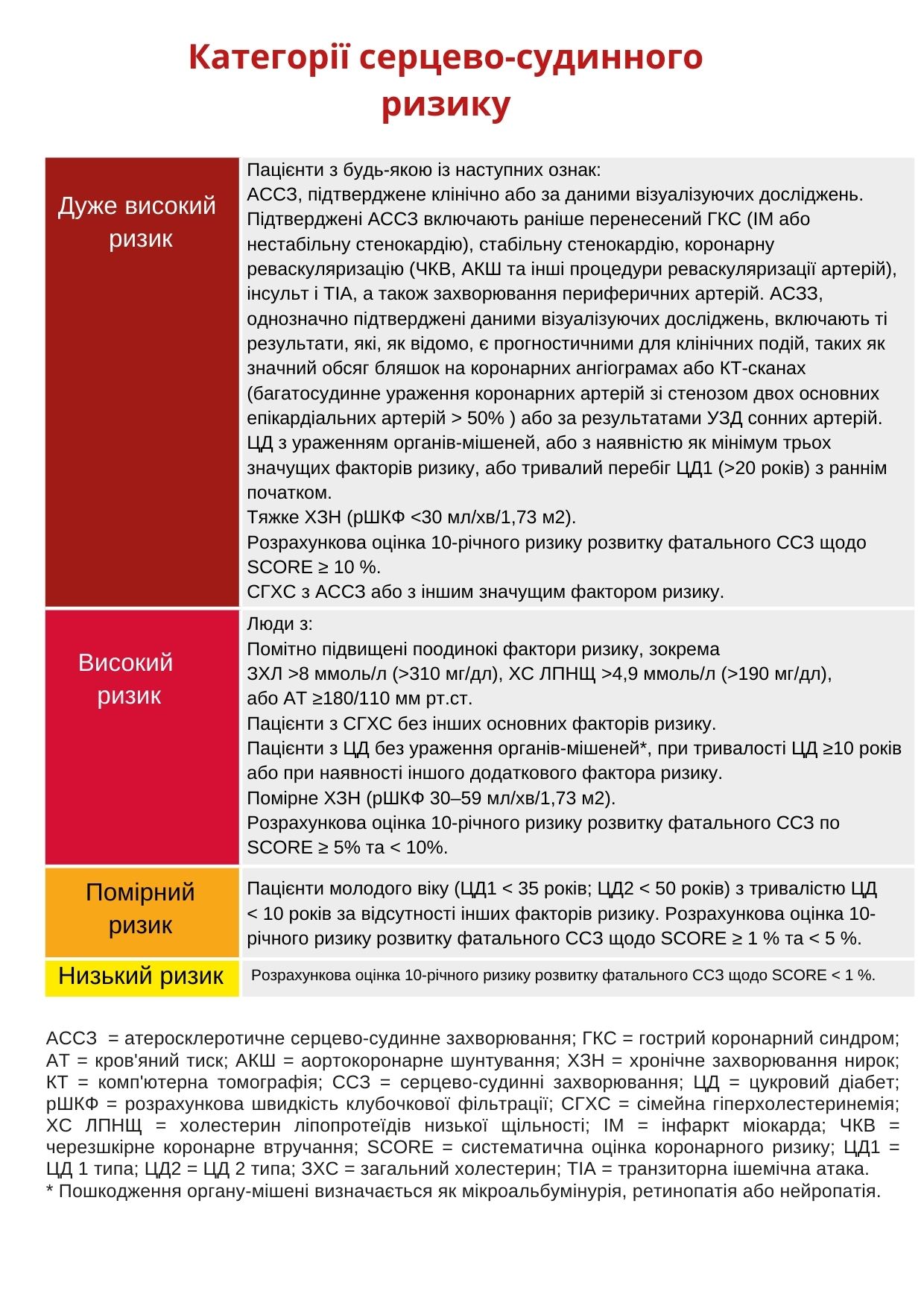
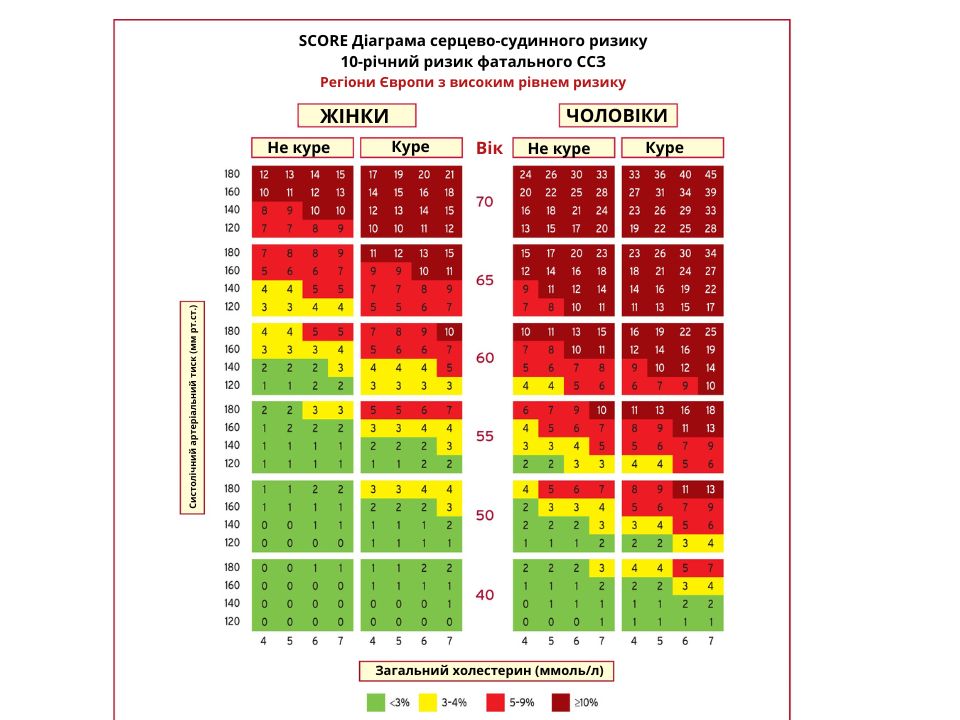
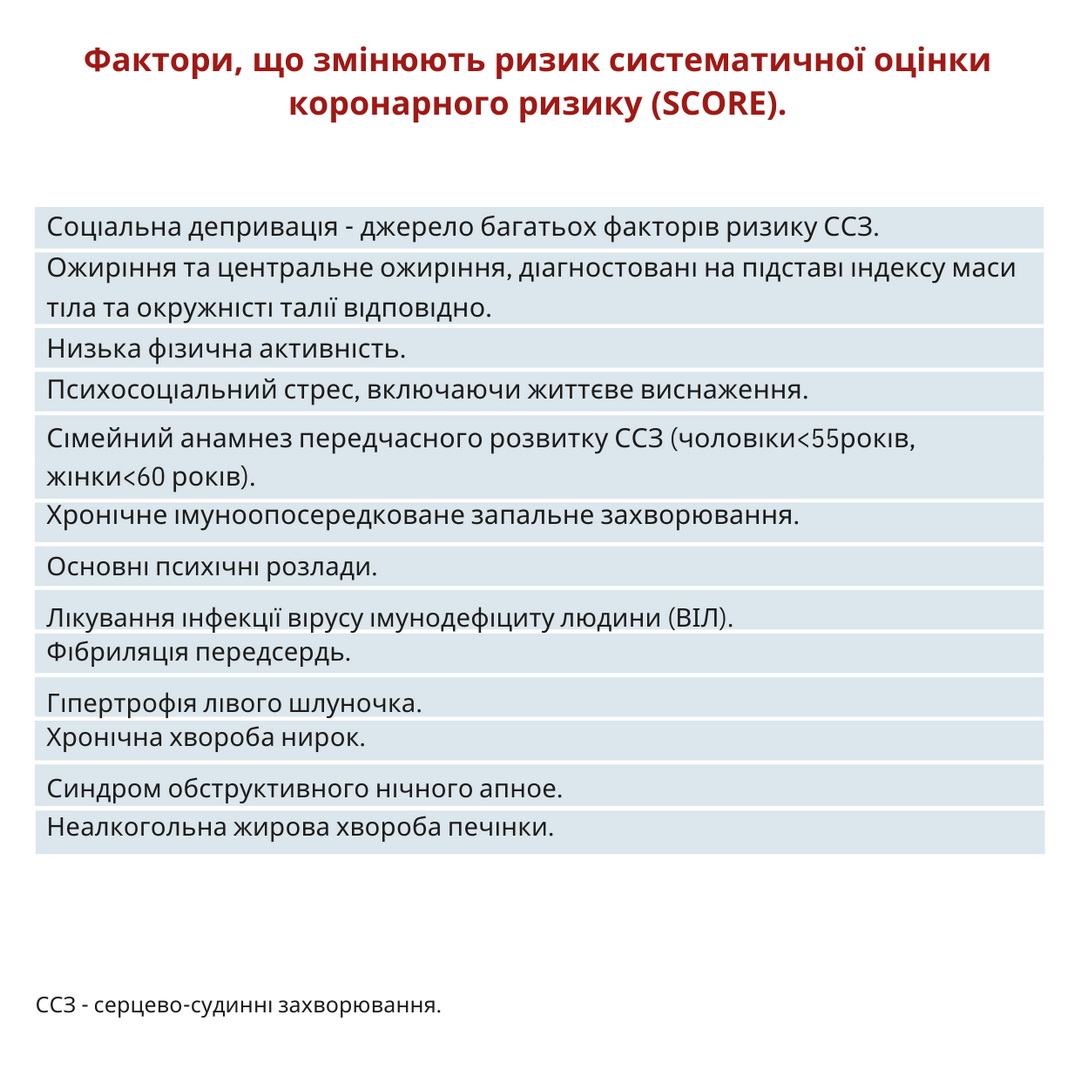
The patient has a history of ASD, which immediately makes him a very high-risk patient (see Table Categories of cardiovascular risk). Without prior MI, the patient would be at high risk with a 6% risk of death from CVD over 10 years based on SCORE. But the presence of abdominal obesity, high TG, low HDL and high Lp(a) increase its risks (see Table Factors that change the risk of SCORE), so SCORE underestimates all the risks.
Treatment
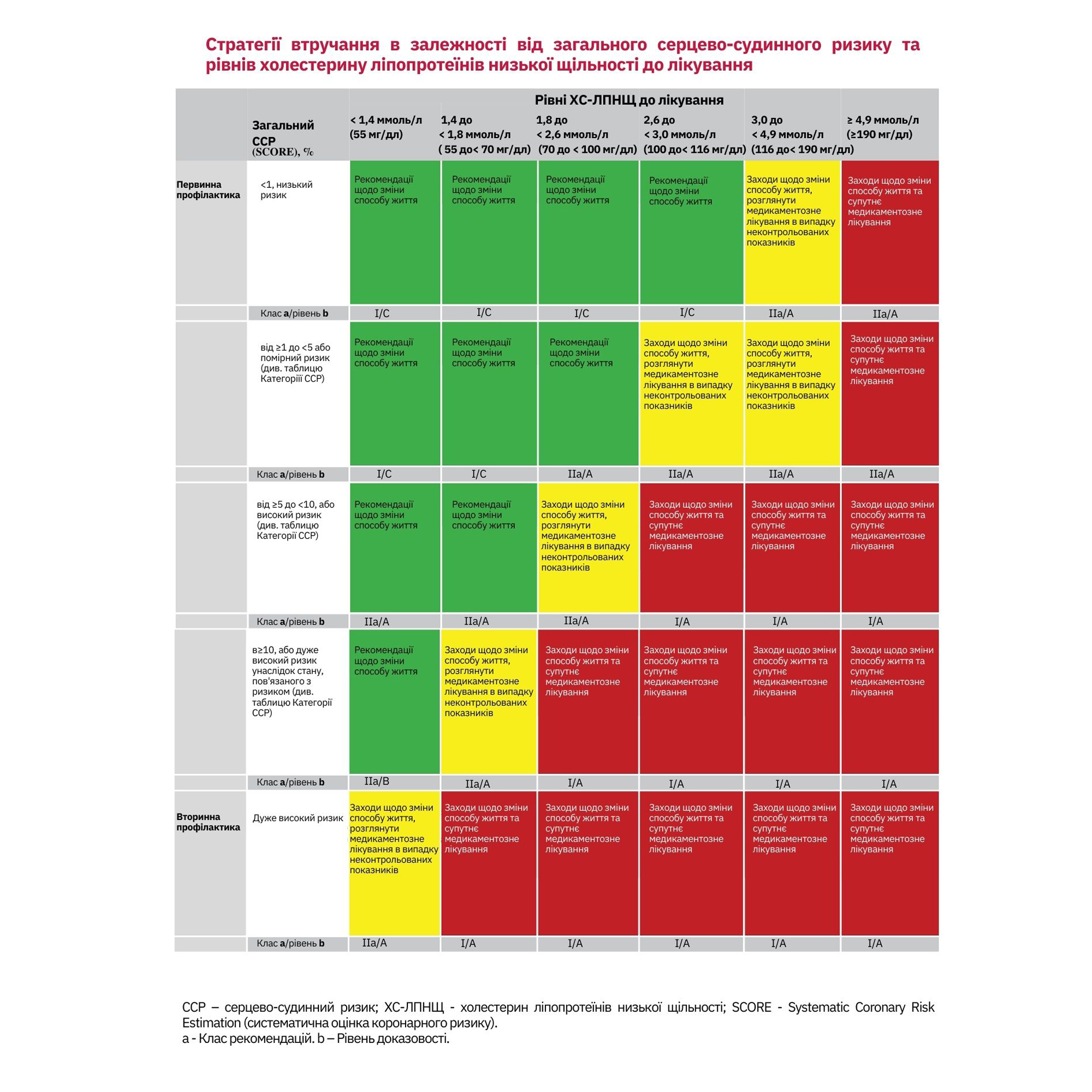
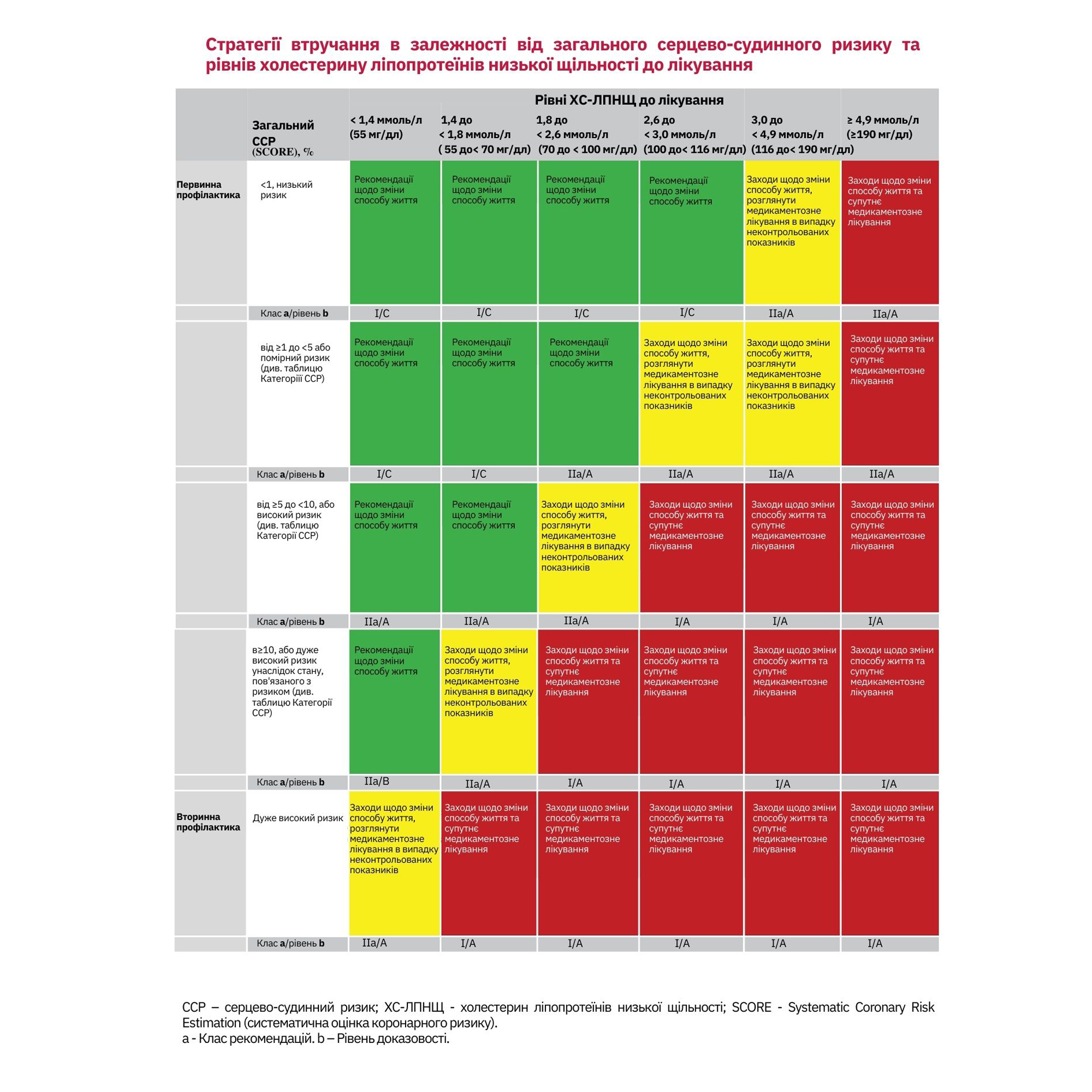
For recommendations, see Table Lifestyle change and concomitant medication intervention.
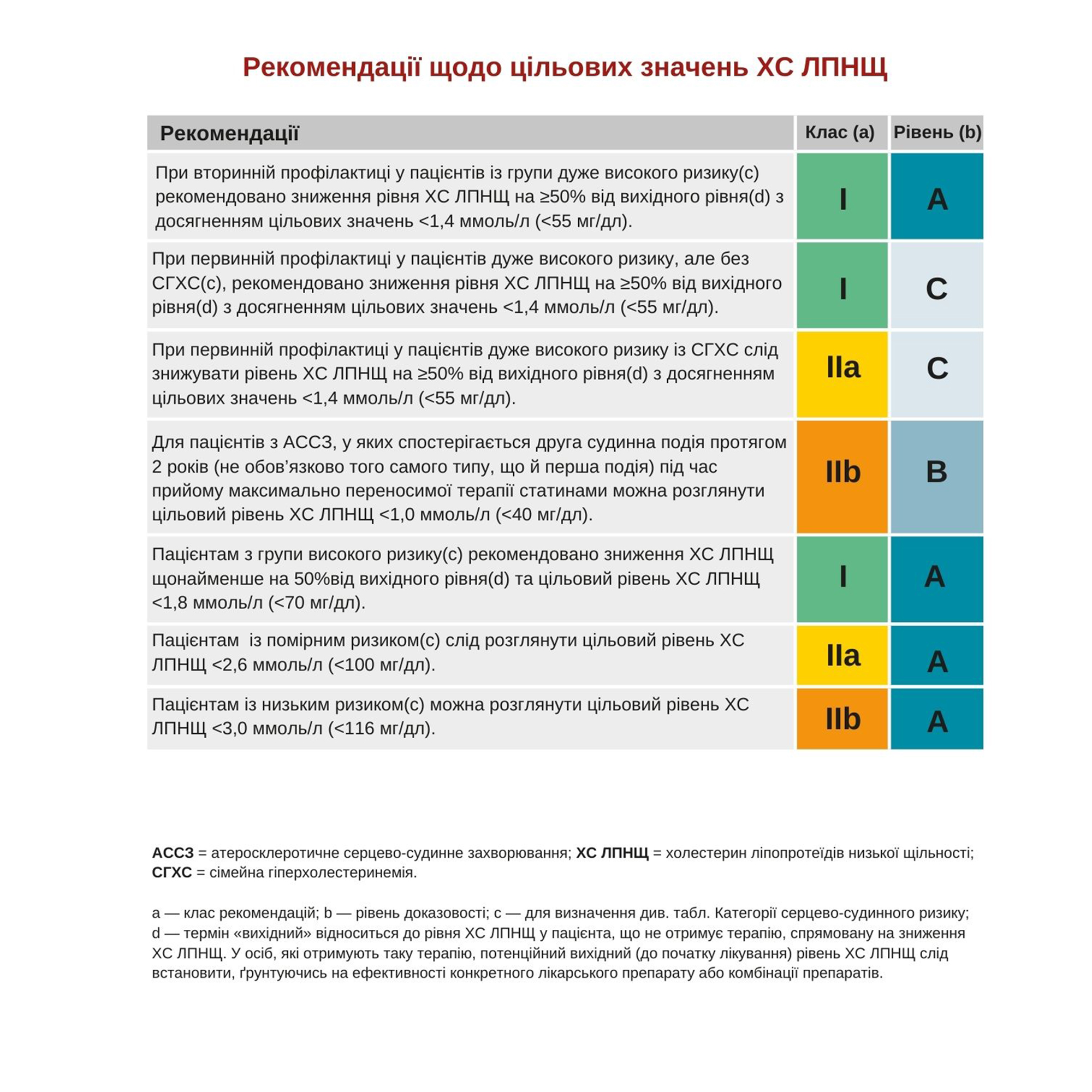
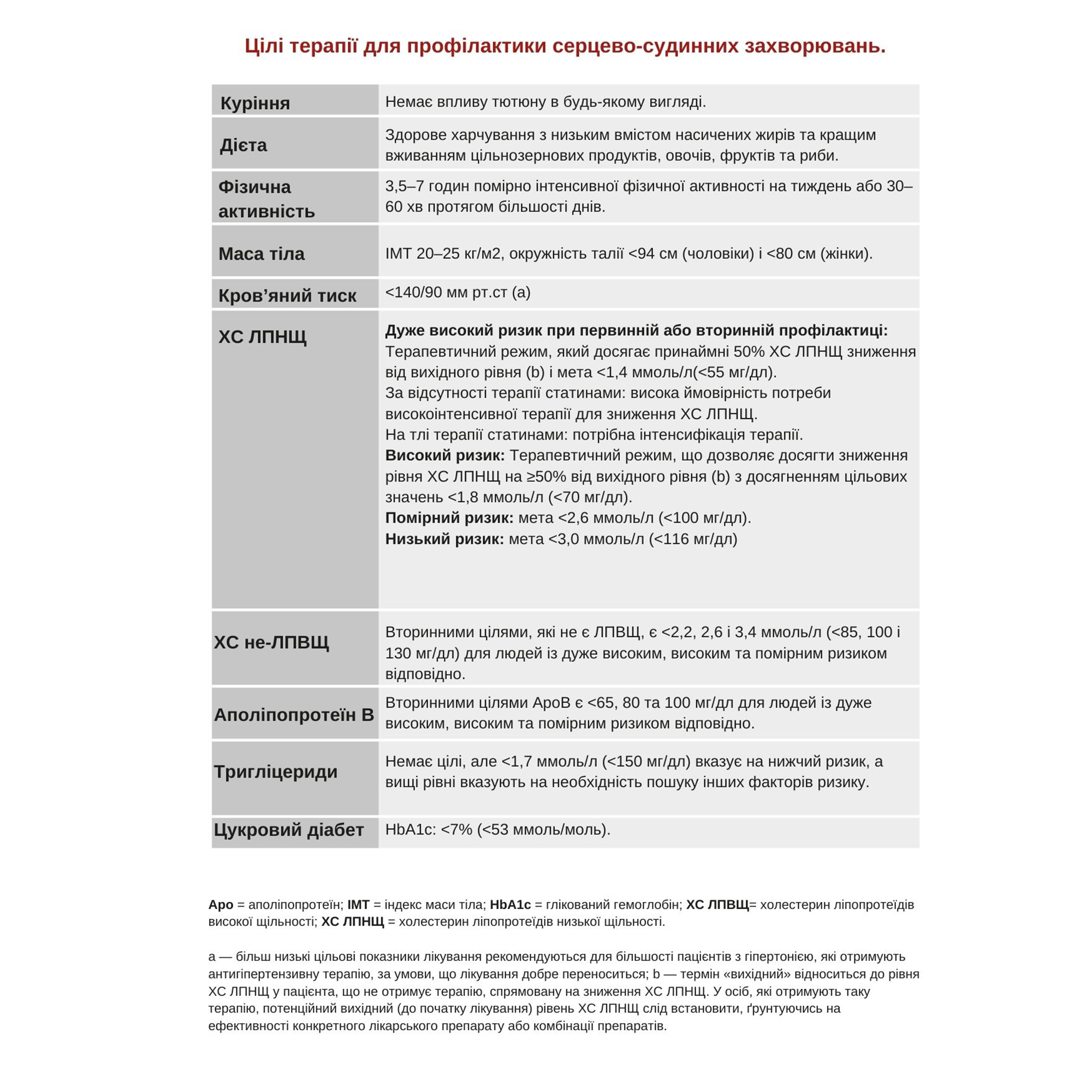
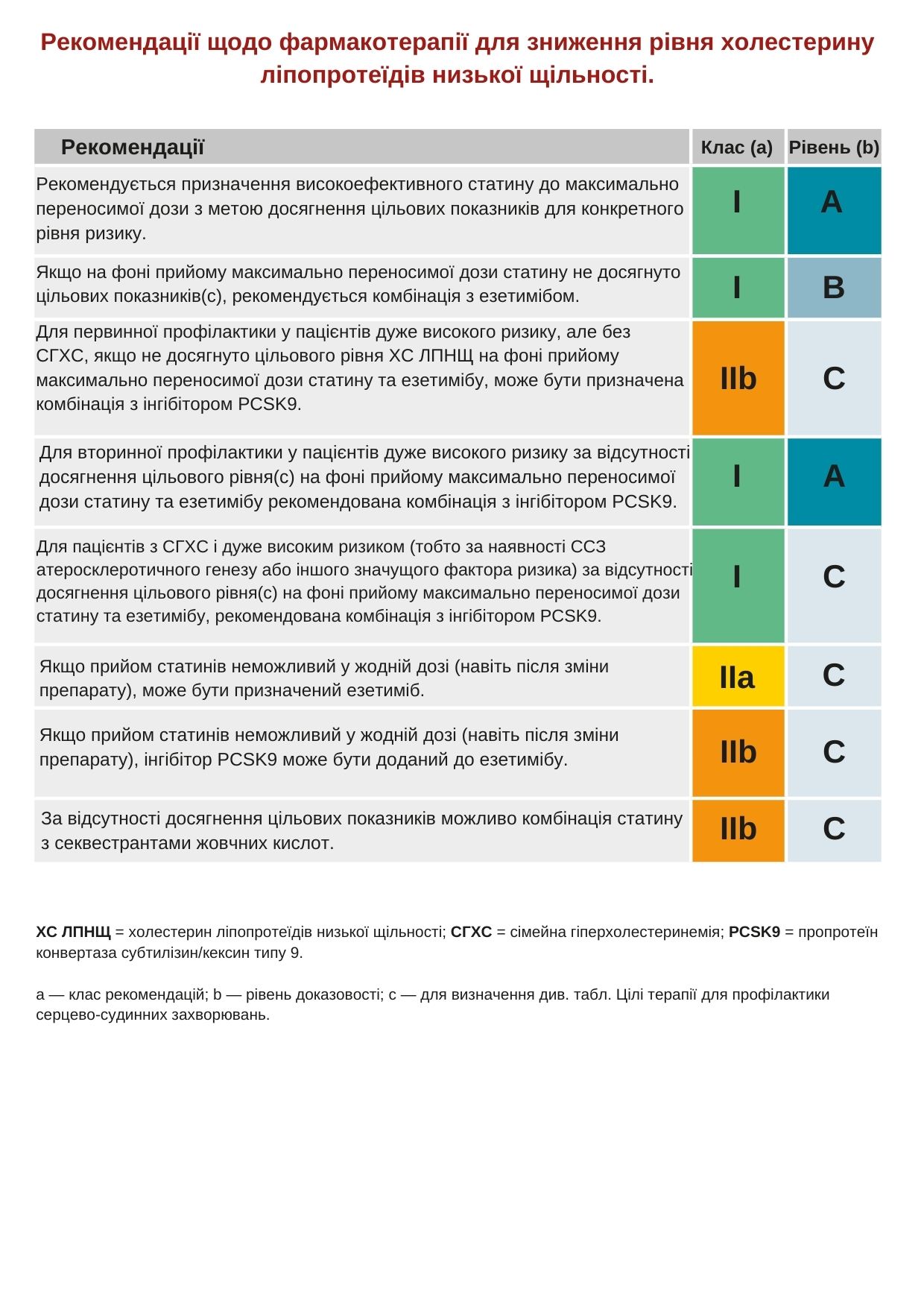
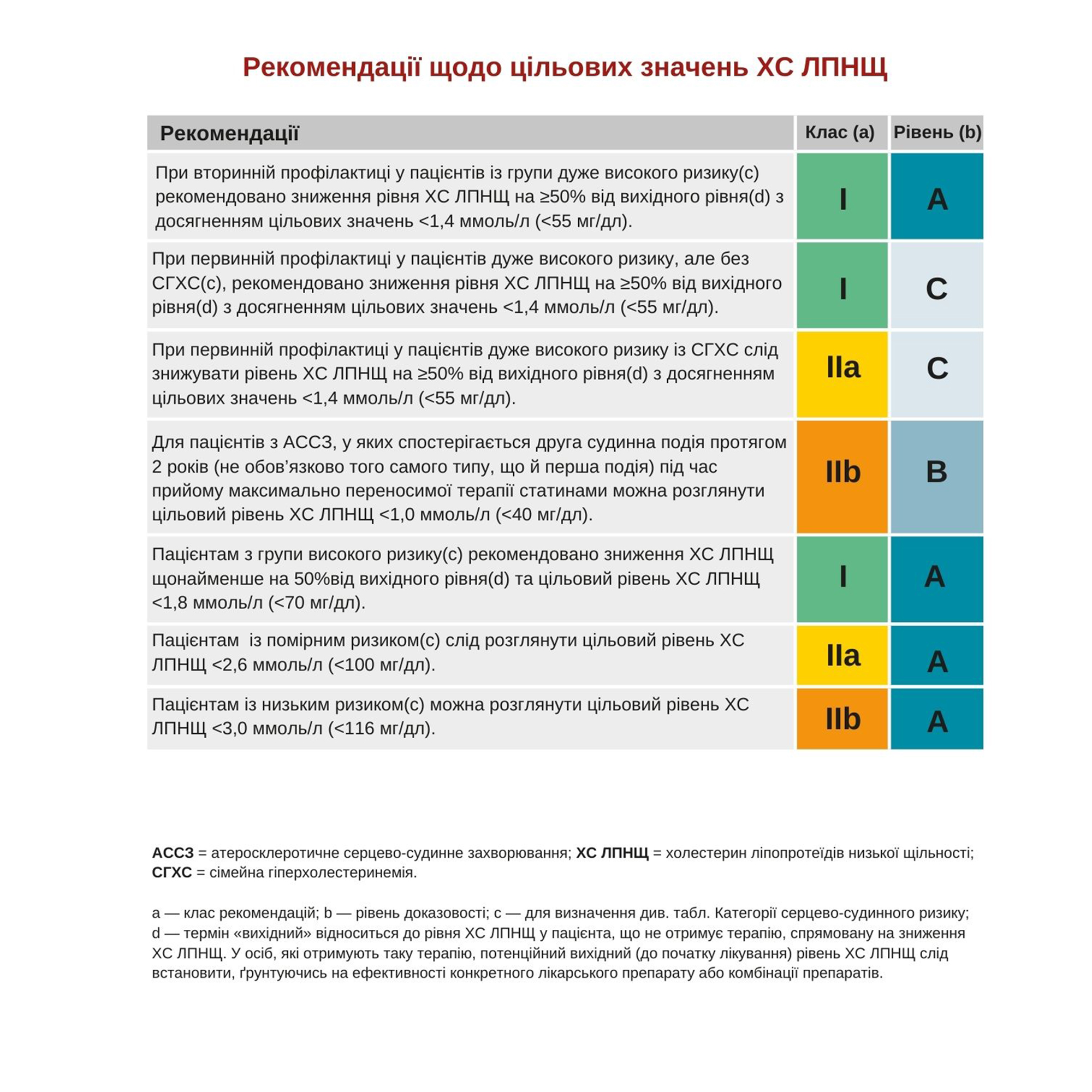
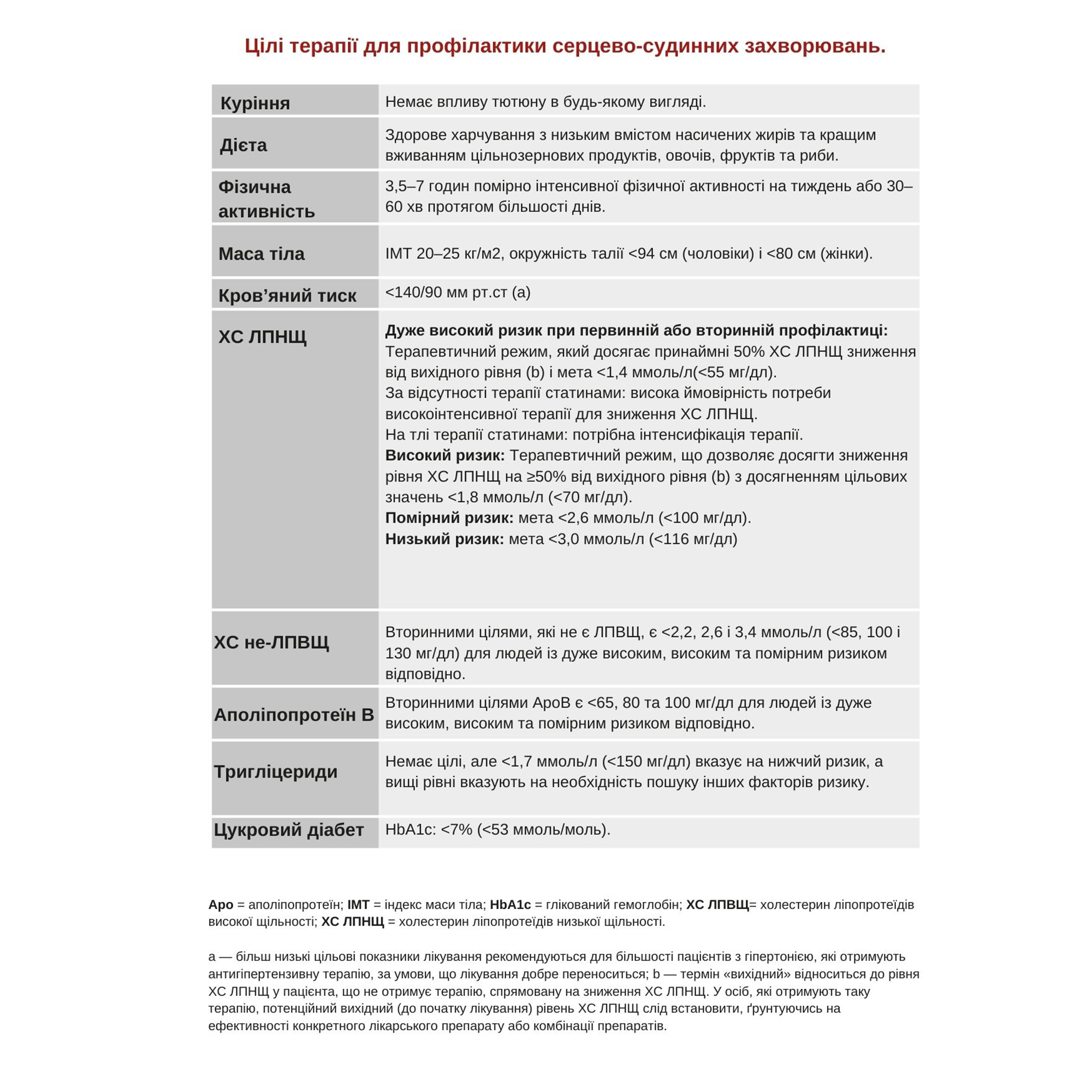
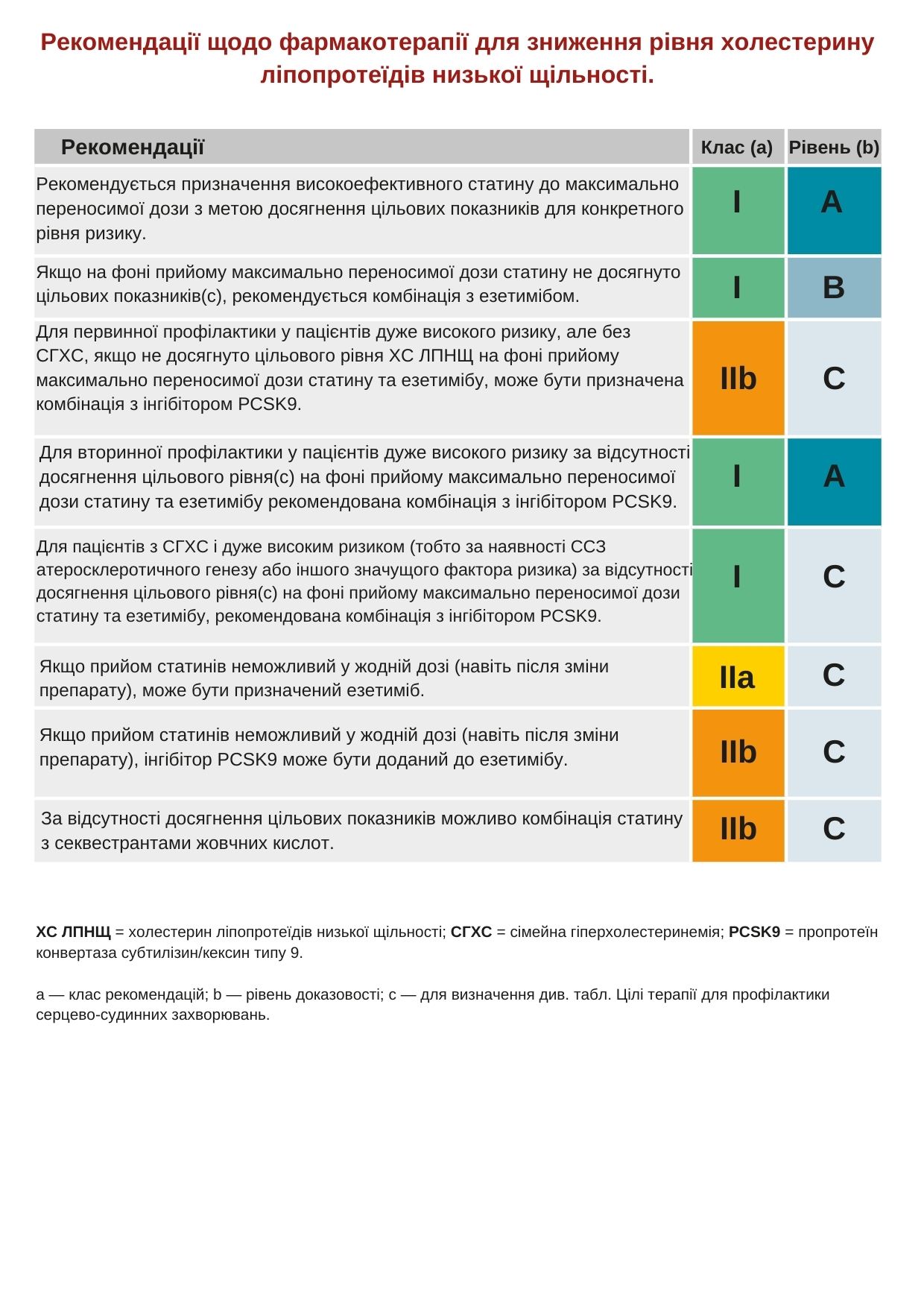
In addition to pharmacological treatment, you should change your lifestyle. These include: quitting smoking, increasing physical activity, losing weight, and striving for a healthier diet. The target LDL cholesterol level is below 1.4 mmol/L (<55 mg/dL) (see table Recommendations for target values of LDL cholesterol and table Treatment goals for the Prevention of CVD) and a reduction of at least 50% compared to baseline LDL cholesterol levels. To achieve this goal, high-intensity statin treatment is recommended (see table Recommendations for pharmacotherapy to reduce LDL cholesterol). His moderately elevated blood pressure should also be treated.
Measures taken
Smoking cessation program, diet recommendations and information about physical activity, preferably, if available, group classes.
Treatment started: atorvastatin 80 mg once a day (once) and an angiotensin converting enzyme (ACE) inhibitor (enalapril 5 mg / day).
Follow-up after 6 weeks.
The patient quit smoking, but did not lose weight.
Blood PRESSURE 135/85mmhg
TC 3.6 mmol/L (139 mg/dl)
TG 2.0 mmol/L (177 mg/dl)
HDL CHOLESTEROL 1.0 mmol/L (38 mg/dl)
LDL CHOLESTEROL 1.6 mmol/L (61 mg/dl)
The patient achieved a 50% reduction in LDL-C, but still did not reach the goal, that is, below 1.4 mmol/L (<55 mg/dl).
According to the recommendations (see Table. Recommendations for pharmacotherapy to reduce the level of LDL cholesterol), ezetimibe 10 mg / day should be added.
The next observation after another 6 weeks.
The patient still does not smoke. He tolerates medications well and has lost 1 kg.
TC 3.4 mmol/l (131 mg/dl)
TG 1.9 mmol/L (168 mg/dl)
HDL 1.1 mmol/L (42 mg/dl)
LDL 1.4 mmol/L (55 mg/dl)
Since this patient initially had a high TG, we should also consider apoB; the target for this patient is <65 mg/dl.
The following observation
After the patient has reached his goal, further monitoring of risk factors may be limited to once a year. However, compliance with all recommendations can be improved with more careful monitoring and a more detailed discussion with the patient of his risk factors.
CASE1. A very high-risk patient in secondary prevention.
Recall! The cases are based on real cases and clinical experience.
Background data
The patient is a 60–year-old entrepreneur, married, has three adult children. He has been smoking 10 cigarettes a day for many years. I came to the hospital for a health check at the insistence of my wife.
What do we need to know to assess its risk?
Medical history
The patient suffered a subendocardial myocardial infarction (MI) 5 years ago. He was sent under the supervision of his therapist, but was not observed. He is currently not taking medication and has no family history of early cardiovascular disease. There is no history of chest pain.
Risk factors
Smoker, body mass index (BMI) 29 kg/m2, waist circumference 105 cm, low physical activity.
Physical status: moderate abdominal obesity. There is no Xanthe. Auscultation of the heart is normal. Arterial pressure (BP) is 145/90 mmHg. Peripheral blood circulation is normal.
Laboratory tests
There were no signs of the previous one on the ECG.
TC 5.2 mmol/L (200 mg/dl)
TG 2.2 mmol/L (193 mg/dl)
HDL CHOLESTEROL 1.0 mmol/L (38 mg/dl)
LDL CHOLESTEROL 3.2 mmol/l (123 mg/dl)
Blood glucose 6.9 mmol/l (124 mg/dl); Lp(a) 200 mg/dl.
What risk category does the patient belong to?
The patient has a history of ASD, which immediately makes him a very high-risk patient (see Table Categories of cardiovascular risk). Without prior MI, the patient would be at high risk with a 6% risk of death from CVD over 10 years based on SCORE. But the presence of abdominal obesity, high TG, low HDL and high Lp(a) increase its risks (see Table Factors that change the risk of SCORE), so SCORE underestimates all the risks.
Treatment
For recommendations, see Table Lifestyle change and concomitant medication intervention.
In addition to pharmacological treatment, you should change your lifestyle. These include: quitting smoking, increasing physical activity, losing weight, and striving for a healthier diet. The target LDL cholesterol level is below 1.4 mmol/L (<55 mg/dL) (see table Recommendations for target values of LDL cholesterol and table Treatment goals for the Prevention of CVD) and a reduction of at least 50% compared to baseline LDL cholesterol levels. To achieve this goal, high-intensity statin treatment is recommended (see table Recommendations for pharmacotherapy to reduce LDL cholesterol). His moderately elevated blood pressure should also be treated.
Measures taken
Smoking cessation program, diet recommendations and information about physical activity, preferably, if available, group classes.
Treatment started: atorvastatin 80 mg once a day (once) and an angiotensin converting enzyme (ACE) inhibitor (enalapril 5 mg / day).
Follow-up after 6 weeks.
The patient quit smoking, but did not lose weight.
Blood PRESSURE 135/85mmhg
TC 3.6 mmol/L (139 mg/dl)
TG 2.0 mmol/L (177 mg/dl)
HDL CHOLESTEROL 1.0 mmol/L (38 mg/dl)
LDL CHOLESTEROL 1.6 mmol/L (61 mg/dl)
The patient achieved a 50% reduction in LDL-C, but still did not reach the goal, that is, below 1.4 mmol/L (<55 mg/dl).
According to the recommendations (see Table. Recommendations for pharmacotherapy to reduce the level of LDL cholesterol), ezetimibe 10 mg / day should be added.
The next observation after another 6 weeks.
The patient still does not smoke. He tolerates medications well and has lost 1 kg.
TC 3.4 mmol/l (131 mg/dl)
TG 1.9 mmol/L (168 mg/dl)
HDL 1.1 mmol/L (42 mg/dl)
LDL 1.4 mmol/L (55 mg/dl)
Since this patient initially had a high TG, we should also consider apoB; the target for this patient is <65 mg/dl.
The following observation
After the patient has reached his goal, further monitoring of risk factors may be limited to once a year. However, compliance with all recommendations can be improved with more careful monitoring and a more detailed discussion with the patient of his risk factors.